NIS 5.2 billion
The Effect of Food Rescue on Food Security and Healthcare Costs in Israel
According to the WHO, a healthy diet includes vegetables, fruit, legumes, unprocessed grains, less than five grams of salt per day, as little added sugar as possible, and unsaturated fats rather than saturated fats. WHO notes that due to changes in lifestyles, increased urbanization, and the proliferation of processed foods, people today tend to consume less fresh fruit and vegetables, and more foods that are high in calories, with added sugar and salt (34).
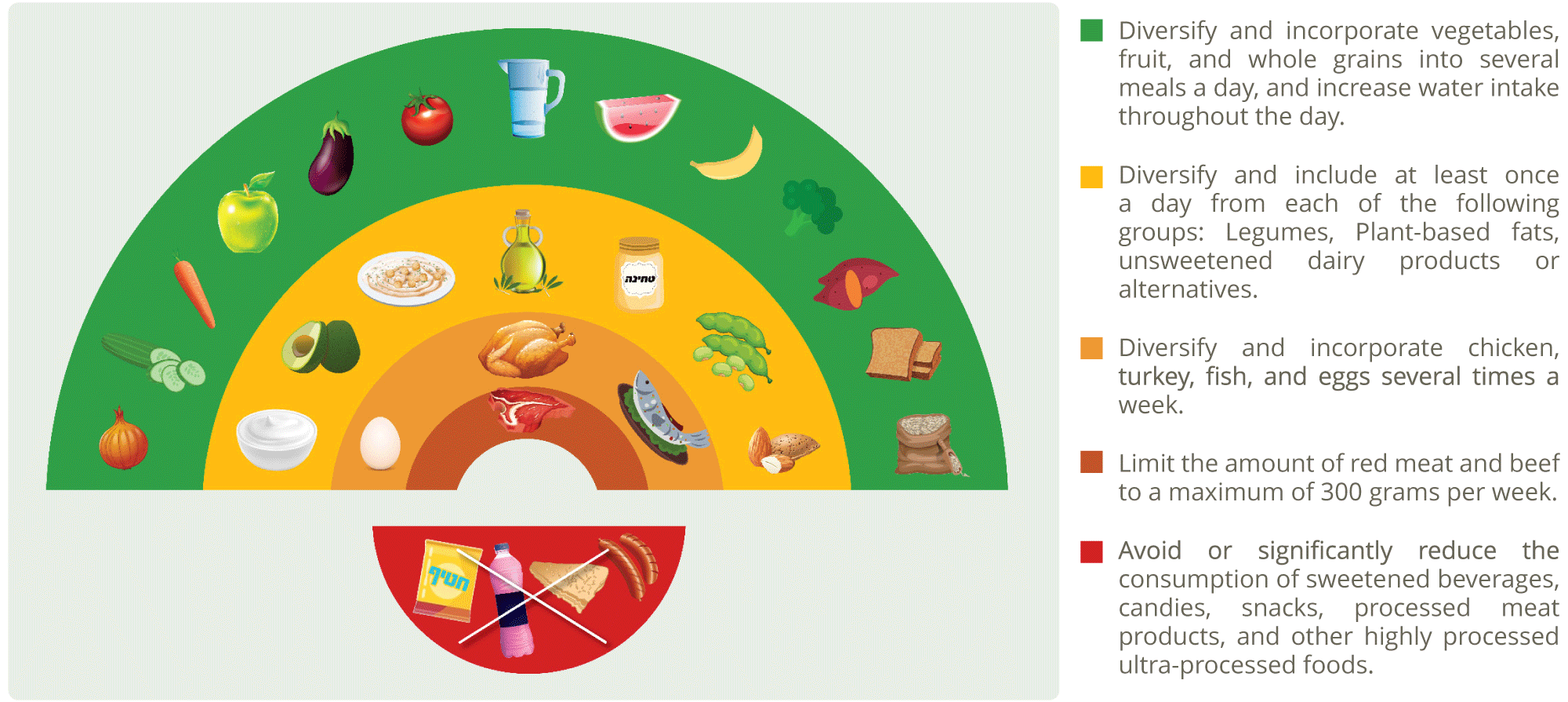
The national nutrition guidelines issued by the Israeli Ministry of Health (35) recommend a diet based on Mediterranean diet principles, rich in a variety of unprocessed plant-based foods including vegetables, fruit, legumes, whole grains, olive oil, nuts and seeds, and a combination of animal-based foods, such as eggs, chicken, and fish. The Ministry of Health recommends reducing the consumption of highly processed foods (foods that have undergone industrial processing and often contain extracted food components or additives). Although processed foods are widely available and convenient, a diet based on them is unhealthy and has been linked to a range of ailments, including obesity, increased risk of chronic illnesses and cancer, a change in the microbiome, and more (36). The Ministry of Health’s recommendations, reflected in the concept of the “food rainbow,” have health, environmental, social, and economic benefits.
Historically, many countries have instituted policies to combat food insecurity that focus on the availability of a sufficient number of calories, not on the quality of the diet. Such policies prioritize sufficient daily caloric intake, without taking into account the quality, composition, or nutritional value of the food consumed. Globally, this policy has been a success, in that it has resulted in a decreased rate of malnutrition, from 12.3% in 2005 to 9.8% in 2021. Thanks to this policy, most of the world’s population can now receive the necessary basic caloric intake.
The food rainbow, Israel's national nutritional recommendations
However, according to the WHO and the FAO, although this policy was successful in reducing the global rate of malnutrition, it did not promote a healthy diet. In fact, it was sometimes in complete opposition to national and international nutritional recommendations. This policy encouraged food-producing systems to develop in such a way that the cost of a healthy food basket is now up to five times more expensive than a “basic food basket” (a term for the food that can be stored or produced throughout the year, and contains a high number of calories in relation to its price). A basic food basket provides an individual with the necessary number of daily calories, but not the variety of food or the nutrients a person needs to be healthy.
In other words, this global policy focused on the supply of daily calories to be consumed, rather than on a supply of varied and nutritious food. Variety of food is just as important as quantity. Fruit and vegetables are a significant component of a healthy diet because they contain many essential nutrients. A diet rich in vegetables and fruit may lower blood pressure, have a positive effect on blood sugar levels, prevent certain types of cancer, and reduce the risk of heart disease, stroke, eye problems, and digestive problems (37). A healthy diet is important for preventing non-communicable diseases (NCDs), such as diabetes, hypertension, heart disease, kidney disease, and depression. NCDs are responsible for 74% of all deaths – 41 million a year, including 17 million under the age of 70 (38). Often, households experiencing food insecurity have diets consisting largely of unhealthy food products.
A study conducted in the UK (39) examined the relationship between food security status and consumption of fruit and vegetables and found that food security status is a significant predictor of fruit and vegetable consumption. For every one-unit increase in the food security score (i.e., more precarious food security), there was an 11% decrease in the incidence of high fruit and vegetable consumption. Thus, the population suffering from food insecurity is also at a higher risk of health problems such as fatigue and frailty, cardiovascular diseases, hypertension, osteoporosis, anemia, birth defects, premature birth, and obesity (40).
Likewise, ongoing food insecurity causes a deterioration of mental health, psychological distress, depression, and anxiety. Moreover, children from food-insecure families often lack access to medical care. An inadequate diet causes cognitive damage that affects children’s learning, memory, thinking skills, and overall damage to well-being. Poor nutrition during critical periods of the development of a fetus or young child can cause developmental delays, which may be apparent among preschool and kindergarten-aged children. Food insecurity impairs concentration in school and increases the likelihood of poor academic achievement and dropping out of educational frameworks early. Compared to children growing up in families with food security, these children may suffer from low psychosocial functioning, and exhibit symptoms such as aggression, hyperactivity, or apathy (41).
The US White House recently published the Biden-Harris Administration National Strategy on Hunger, Nutrition, and Health, which states that on a personal level, food insecurity poses a risk factor for chronic physical and mental illness, decreased academic achievement, diminished earning capacity, and financial distress. On a national level, food insecurity leads to an increase in healthcare expenses and reduces productivity. Accordingly, the White House Report recommends a shift from addressing the problem of hunger to addressing the problem of food insecurity and poor nutrition. It clearly states that financial access to a healthy food basket, which ensures adequate nutrition essential for physical, emotional, and cognitive functioning, is necessary for realizing food security.
However, the current high cost of healthy food in relation to disposable income limits access to a healthy food basket in both rich and poor countries. Therefore, rescuing healthy food products and distributing them to people in a state of food insecurity, who are unable to purchase and consume enough healthy food, can help ensure adequate nutrition, improve their health, and therefore reduce healthcare expenses for the national economy.
In general, the healthcare systems in developed countries around the world include a combination of public and private entities, in terms of their funding and organization. State-owned public hospitals, and hospitals owned by non-profit organizations, operate alongside private for-profit hospitals and even compete with them. Public healthcare facilities may also provide private services to patients. Physicians and other healthcare professionals may work in public or private settings, and some combine the two.
Most Western countries provide their citizens with universal health insurance, alongside the option to voluntarily purchase private insurance. Healthcare services are funded by general or designated state taxes, as well as from citizens’ pockets, in the form of direct expenses and co-payments (42). The public-private mix of spending on healthcare varies between countries. Some tend towards a higher rate of public financing of the healthcare system, while in other countries, primarily the United States, a significant portion of healthcare costs are paid for privately.
Analysis of the proportion of government spending, out of the total spending on healthcare in Western countries, shows that in the US, public spending is relatively low, only about 55%, while a significant portion of healthcare spending is paid for privately. In both Israel and Canada, about 70% of healthcare costs are funded by the government (43).
Additionally, healthcare spending as a percentage of per capita GDP in the US is particularly high, about 17%. In Canada the corresponding figure is about 11%, while in Israel it is about 8%.
Increased healthcare expenses resulting from poor nutrition and food insecurity
Although the FAO study indicates that consuming a healthy food basket with plentiful fruit and vegetables is expensive, and may cost up to five times more than a basic food basket, this chapter will demonstrate that an unhealthy diet may be even more expensive.
Studies and projections from around the world have indicated that unhealthy diets and food insecurity are related to increased expenses both for public healthcare systems and for private individuals. The studies link these increased costs to health conditions that are related to living in a state of food insecurity, and which would not have occurred if the same person had food security. These expenses include hospitalizations, emergency room visits, doctors’ appointments, purchasing medications, etc.
A study conducted in the US in 2016 reviewed a set of studies published between 2005 and 2015 that evaluated the relationship between food insecurity and various diseases (44). It found that food insecurity is related to about 4% of self-reported cases of arthritis, about 6% of reports of diabetes, about 15% of reports of dental problems, about 13% of reports of vitamin deficiency, about 7% of reports of obesity, about 11% of reports of mental disorders, about 30% of reports of depression among adults and about 34% of prescription drugs for children.
In another study from the US published in 2019, researchers focused on the relationship between levels of households’ food insecurity and their health expenditures. Using data from the National Health Interview Survey (NHIS) and the Medical Expenditure Panel Survey (MEPS), they estimated the additional healthcare costs that are linked to food insecurity in various states and regions within the US (45).
Poor nutrition is the biggest spender of the NHS* budget
The researchers concluded that annual expenditures on healthcare services among the adult population (ages 18 and older) living in food insecurity are higher by approximately $2,030 per person (46), as compared to adults who have food security.
A study conducted in the United Kingdom found that about 46% of the expenses for the country’s National Health Service (NHS) are linked to poor nutrition, lack of physical activity, smoking, alcohol consumption, and obesity. The NHS annually spends approximately GBP £43b ($52b), and of this, approximately GBP £6b ($11.5b) are linked to diseases resulting from poor nutrition, including metabolic and endocrine problems, cancer and cardiovascular diseases. This is higher than for any other factor examined in the study (47).
A longitudinal study conducted in Australia over 15 years found that the health expenses of women who regularly ate fruit and vegetables were lower than those who did not (48). The authors assessed that subsidizing fruit and vegetables and raising taxes on unhealthy food could potentially yield an annual savings of AUD $3.4b (USD $2.3b) for Australia’s healthcare system.
A study conducted in Canada, published in 2015, examined the relationship between food insecurity and health costs of the population in the province of Ontario, aged 18-64. The researchers examined the link between this population’s food security status (assessed according to data from a community health survey) and data on administrative healthcare costs, in order to determine the medical treatment costs for the population over the course of 12 months. The study, published in The Canadian Medical Association Journal, showed that total healthcare costs, and the average costs for hospital admissions, emergency department visits, physician services, same-day (emergency) surgeries, home care services, and prescription drugs, rose systematically as household food insecurity worsened (49).
Additional annual per capita healthcare costs resulting from food insecurity in Ontario, Canada (in USD)
The study found that the more severe the level of food insecurity, the higher the health expenses. The average additional annual cost of healthcare costs for an adult living with food insecurity in Ontario was found to be CAD $1,224 (50). (USD $907)
The increased costs were primarily attributed to three factors: hospitalizations, the purchase of medications, and physician services. The researchers concluded that household food insecurity is a strong predictor of the use of healthcare services and healthcare costs for working-age adults, independent of other social factors that affect health. They stated that government interventions to reduce food insecurity could significantly offset public expenditures on healthcare.
FAO data show that the problem of food insecurity in Israel is among the most serious in the world. While the poverty rate in Israel is similar to that in the US, the food insecurity rate in Israel is 1.7 times higher. This means that the burden on Israel’s healthcare system as a result of food insecurity is greater than in any other country.
To estimate the additional national healthcare costs that result from food insecurity in Israel, data pertaining to the healthcare systems in Canada, the US, and Israel were compared. The findings show that Canada is a more relevant country for comparison to Israel, regarding expenditures on healthcare. Canada and Israel have similar rates of public spending on healthcare, and spending on healthcare as a percentage of GDP (51). In the US, public spending on healthcare is significantly lower, while the percentage of the GDP spent on healthcare is significantly higher, as compared to Israel or Canada. Therefore, the US cannot be used as a relevant reference point for Israel, regarding national healthcare expenditures. Since the analysis indicated that Canada is a relevant comparison country for Israel in relation to healthcare expenditures, the annual health expenditures per capita in these two countries were compared. Analysis of World Bank data on annual healthcare expenditures shows that per capita spending on healthcare is about 20% higher in Canada than in Israel (52).
In the above-cited study, the additional annual per capita healthcare costs due to food insecurity in Canada were assessed at CAD $1,224 (USD $907). To make a comparison with Israel, a downward correction of approximately 20% is necessary. Following this adjustment, it appears that the additional annual per capita healthcare cost due to food insecurity in Israel is approximately $980 (about NIS 3,700).
According to the analysis presented in this Report, about 1.4 million people (53) in Israel live with food insecurity. The total excess healthcare cost to the Israeli economy from food insecurity is assessed at NIS 5.2b ($1.47b) per year, equivalent to about 5% of national healthcare expenditures (54).
Annual health expenditure per capita
This Report examined the economic impact of food insecurity in terms of excess healthcare costs in Israel. This chapter focuses on the direct impact food insecurity has on healthcare costs in Israel for 2022. Other indirect economic costs related to food insecurity were not measured.
Bread for the World, a US-based anti-hunger organization, assessed the indirect impacts of food insecurity, such as missing work days as a result of illness or caring for ill relatives, costs of special education in public primary and secondary schools for children living with food insecurity, and the costs of school dropout. They estimated that in 2016, these costs were approximately $24 billion; an additional 16% over the direct costs of food insecurity that were assessed in the study (55).
Other indirect effects of food insecurity were described in a report by the Second Harvest North Central Food Bank, including: poor cognitive and physical development of children with iron deficiency, increased risk of birth defects, development or exacerbation of mental illness, and the risk of suicide due to hunger and poor nutrition (56).
Additional annual health costs per capita from food insecurity
Therefore, the assessment presented in this chapter of the direct healthcare costs that result from food insecurity is not exhaustive. It serves as a basis for future assessments of the total economic cost of food insecurity in Israel.
However, even this partial assessment makes it clear that rescuing healthy food and providing it to the population experiencing food insecurity – who do not usually purchase and consume healthy food – may enable them to improve their nutrition and health, which will reduce healthcare costs to the national economy.